Colorectal Cancer
Colon cancer forms in the tissues of the colon (large intestine). Rectal cancer forms in the tissues of the rectum, which is the last several inches of the large intestine before the anus. Either of these cancers is called colorectal cancer.
In the United States, colon cancer is the third deadliest form of cancer. According to the American Cancer Society, about 150,000 people are diagnosed with colon cancer and about 50,000 people die from colon cancer each year.
Please make these links to the headers:
- Preventing Colon Cancer
- Colon Polyps
- Risk Factors
- Warning Signs and Symptoms
- Treatments and Procedures
Preventing Colon Cancer
Getting screened is the first step in preventing colon cancer. Regular colonoscopies should begin at age 45 for adults who do not have increased risk factor for colon cancer. Individuals that do have increased risk factors may need to have a colonoscopy earlier than age 45. Anyone with increased risk factors should consult with their healthcare provider to determine at what age a screening colonoscopy should be done.
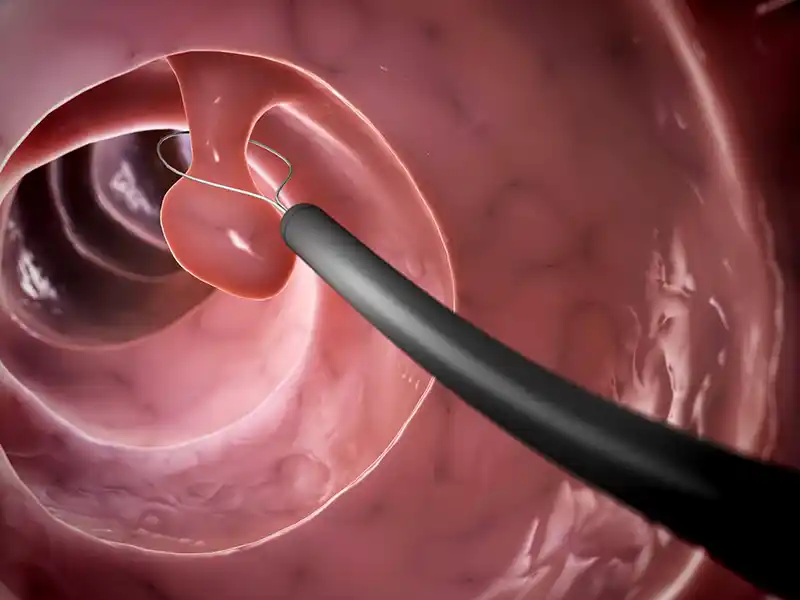
The purpose of a screening colonoscopy is to find and remove colon polyps (make link to colon polyps header below) to decrease the risk of colon cancer.
Colon Polyps
A colon polyp is a growth of extra tissue in the lining of the colon (large intestine). While some can be cancerous, most are not. However, almost all colon cancers develop from colon polyps. By removing polyps early, the chance of a polyp turning into colon cancer is eliminated.
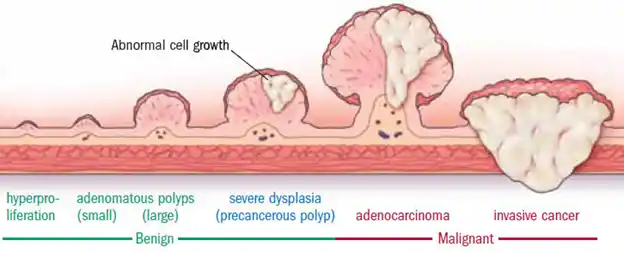
Colon polyps
People with a higher risk for developing polyps are anyone over age 50, those who have had polyps previously or those who have a family history of polyps or colon cancer.
Polyps generally do not cause symptoms. If a patient does have symptoms, they can include: blood in their underwear or on toilet paper after a bowel movement, blood in stool, or constipation or diarrhea that has lasted more than a week.
Most important, however, is that not having a family history of colon cancer, or symptoms, does not protect you. 80 percent of those who are diagnosed with colon cancer have no family history or symptoms.
If polyps are removed through a colonoscopy and performed on the schedule recommended by your physician, the chances of getting colon cancer are dramatically reduced. If precancerous colon polyps are removed, the chance of the polyp turning into cancer is eliminated. If colon cancer is detected early well before symptoms occur it is more than 90 percent curable. Depending on an individual’s medical and family history, colonoscopies are typically recommended every one, three, five or 10 years.
Risk Factors
There are two types of colon cancer risk factors:
Uncontrollable risk factors cannot be changed. The most common uncontrollable risk factors are:
- Age 50 or older
- Racial or ethnic background, including American Indians, Alaska Natives and African-Americans)
- Personal or family history of colorectal polyps or colorectal cancer
- Inflammatory (IBD), such as Ulcerative Colitis or Chron’s disease
- History of radiation to the abdomen or pelvis area
- Having an inherited genetic family cancer syndrome, such as Lynch syndrome or familial adenomatous polyposis (FAP)
Controllable risk factors are risk factors you can change. The most common controllable risk factors are:
- Obesity
- Diabetes
- High-fat diet or a long-term diet high in red meat (such as beef, pork, lamb, or liver) or processed meat (like hot dogs and some lunch meats)
- Smoking
- Alcohol use
- Sedentary lifestyle
Lifestyle changes can also be made to reduce the risk of colon cancer. Take the following steps:
- Add fruits, whole grains and vegetables to your diet
- Limit saturated fat
- Limit alcohol
- Eat a varied diet
- Stop smoking
- Stay active and maintain a healthy body weight
- Add a regular colonoscopy, as prescribed by your physician, to your health-care practices
Warning Signs and Symptoms
Many cases of colon or colorectal cancer have no symptoms or warning signs until the cancer has advanced. Although many conditions and diseases have the same symptoms, patients should consult their doctor if they have any of the following symptoms:
- Abdominal pain or tenderness in the lower abdomen
- Bloody stool, either bright red or very dark
- Diarrhea, constipation or other changes in bowel functions
- Intestinal obstruction
- Narrower than normal stools
- Unexplained anemia
- Unexplained weight loss
- Bloating, fullness or cramps
- Vomiting
Treatments and Procedures
Treatment options for colon cancer depend on the following:
- The stage of the cancer
- Whether the cancer has recurred
- The patient’s general health
If the cancer is small, and has not grown outside of a polyp, it is sometimes possible that it may all be removed during a colonoscopy.
If the cancer has spread outside of a polyp, then there are three primary treatment options available: surgery, chemotherapy and radiation.
Surgery involves removing the portion of the colon (large intestine) that has cancer and rejoining the colon where the cancer was removed. If the healthy portions of the colon cannot be rejoined, then the patient will have a temporary or permanent colostomy bag. A colostomy is done temporarily to give the bowel time to heal before rejoining the health portions of the colon; sometimes it becomes permanent if too much of the colon has to be removed.
Chemotherapy can be used after surgery to destroy any remaining cancer cells, and may be recommended by the doctor if the cancer has spread beyond the colon. Chemotherapy can be used in conjunction with radiation.
Radiation therapy uses powerful energy sources to kill any cancer cells that may remain after surgery or to shrink large tumors before an operation. This option is rarely used in early stages of colon cancer.
