Barrett’s Esophagus
Barrett’s esophagus is a change in the lining of the esophagus (the tube that carries food and liquids from the mouth to the stomach) caused by chronic reflux. Content from the stomach and small intestine flow back (reflux) into the esophagus and cause irritation. This irritation changes the lining of the esophagus and makes it similar to the lining of the stomach and the intestine.
Symptoms
Barrett’s esophagus alone has no signs or symptoms. Because of its close connection with Gastroesophageal reflux disease (GERD), symptoms of GERD are often present and include:
- Heartburn – A burning sensation that can run from your throat to the center of your chest
- Regurgitation of sour liquid or food
- Trouble swallowing (If you’re having trouble swallowing, seek care immediately)
Diagnosis
A doctor may suspect Barrett’s esophagus by reviewing a patient’s medical history, current symptoms, and risk factors. To confirm the diagnosis, doctors perform an upper endoscopy (EGD).
An upper endoscopy is a test that allows a physician to see the inside of the esophagus and stomach using a small lighted tube. After examining the appearance of the esophagus, the doctor may remove small tissue samples (biopsies) to make the diagnosis.
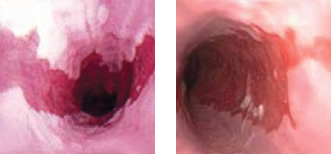
Endoscopic views of Barrett’s Esophagus
The tissue samples that are taken will be sent to a lab and examined by a Pathologist, which is a doctor who is an expert in examining tissue samples. The pathologist will confirm the diagnosis of Barrett’s esophagus when the tissue samples have abnormal, precancerous cell growth (known as dysplasia).
The pathologist will grade the dysplasia into one of three categories:
- No dysplasia: Barrett’s esophagus is present, but there are no precancerous changes
- Low-grade dysplasia: Small changes in cells are present
- High-grade dysplasia: Significant changes in cells are present. Patients with high-grade dysplasia are at higher risk for developing esophageal cancer.
Treatment
The primary goal of treating Barrett’s esophagus is to stope the damage to the esophagus, which is eliminating acid reflux. Acid reflux can be controlled by diet and lifestyle modifications, as well as medications. Your physician may recommend repeating the upper endoscopy on a periodic basis to take tissue samples in order to monitor the dysplasia for any changes. Further treatment would be determined by your physician if those changes occur.
